Abstract
Background: Despite achieving complete remission with standard chemotherapy and allogeneic hematopoietic stem cell transplantation (allo-HSCT), patients with acute myeloid leukemia (AML) are still at high risk of transplant failure due to disease relapse. Maintenance therapy post allo-HSCT including hypomethylating agents or FLT3 inhibitors is implemented in our institutional guidelines to mitigate this risk. Moreover, measurable residual disease (MRD) status of patients is considered an important independent marker of disease prognosis, in which a detectable MRD status pre-transplant is associated with poorer long-term outcomes.
Objective: The aim of this research is to evaluate the impact of maintenance therapy post allo-HSCT on the survival outcomes of transplanted patients based on their pre-transplant MRD status.
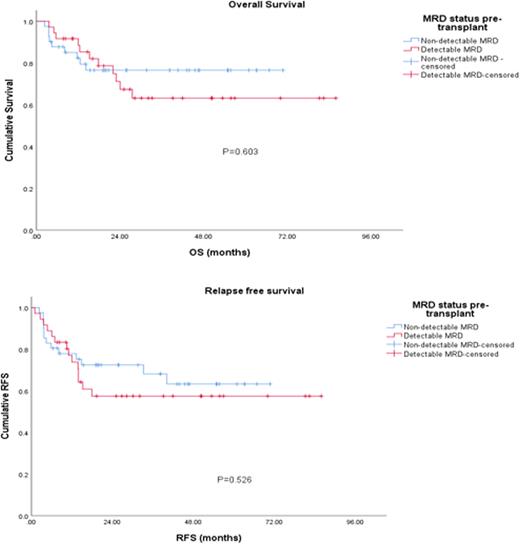
Methods: We performed a retrospective chart review for a total of 108 adult patients diagnosed with AML and who had undergone allo-HSCT at our center between 2015 and 2021. We estimated both overall survival (OS) and relapsed free survival (RFS) using Kaplan Meier curves from the time of transplant among patients who received maintenance treatment based on their MRD status pre-transplant. MRD status was determined using either multiparametric flow cytometry, next-generation sequencing, and/or RT-PCR.
Results: The median age at transplant was 47 years, 60% (n=65) of the patients were males. 66.7% of the patients had an intermediate disease risk index score. 25.2%, 61.8% and 13% of the patients had favorable, intermediate and adverse ELN risk respectively. Among the 108 patients, 77 received maintenance therapy post-transplant, of which 36 patients had a detectable pre-transplant MRD and 41 patients did not. Maintenance therapy consisted mainly of low dose hypomethylating agent (HMA) azacitidine in 68.8% (n=53) of the patients, followed by tyrosine kinase inhibitors (TKI) in 18.2% (n=14) of the patients, and a combination of HMA with TKI, and/ or a BCL2 inhibitor in 13% (n=10). Median duration of maintenance was 20.7 months (range: 0.1-84.2 months). Among patients who received maintenance therapy (n=77), there were no statistically significant difference in both OS and RFS based on MRD status pre-transplant, (4-year OS: 76% versus 63%, p=0.6; 4-year RFS: 63% versus 57%, p=0.53).
Conclusions: Our analysis showed no significant difference in survival outcomes of patients receiving maintenance therapy post allo-HSCT based on their pre-transplant MRD. Maintenance treatment could overcome the negative predictive value of detectable MRD to be confirmed by larger prospective studies.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.